摘要:脊柱透明细胞脑膜瘤(CCMs)作为罕见的硬脑膜来源病变,通常侵袭年轻人群。本文报道了一例极为罕见的形似神经鞘瘤的巨大非硬脑膜来源脊柱 CCM 病例,并进行了详尽的文献综述。通过在 PubMed 和 Embase 数据库检索至 2020 年 1 月 1 日的文献,共发现 19 例非硬脑膜来源脊柱 CCM 报道。从中提取了作者、发表年份、患者与肿瘤特征、治疗方式及预后等相关数据。结果显示,患者发病平均年龄为 20.58 岁,女性占 63.16%(12 例),男性占 36.84%(7 例)。最常见发病部位为腰骶部,占比 79%(15 例)。15 例(79%)肿瘤头尾径≤2 个椎体节段,仅 4 例(21%)≥2 个椎体节段。18 例(95%)患者接受了肿瘤全切除术(GTR),1 例接受次全切除术(STR)。5 例(26.14%)患者出现复发,其中 4 例在术后 6 个月内复发,最早于 STR 术后 2.3 个月出现。本文所报道病例为一名 19 岁男性,诊断为腰骶部硬膜内病变,肿瘤头尾径≥2 个椎体节段,伴有椎间孔延伸及椎体扇贝样改变,行 GTR 术,术中发现肿瘤向椎间孔延伸并与右侧 S1S2 神经根相连,无硬脑膜附着,术后 6 个月随访磁共振成像未见疾病迹象。非硬脑膜来源脊柱 CCM 极为罕见,对于年轻患者出现的巨大硬膜内肿瘤且影像学特征类似神经鞘瘤时,应将其纳入鉴别诊断范畴。该肿瘤好发于年轻患者,常累及多个椎体节段,即便行 GTR 术后,复发与转移风险仍较高,故而需对整个神经系统进行密切随访。
关键词:透明细胞脑膜瘤;硬膜内肿瘤;非硬脑膜来源脑膜瘤;神经鞘瘤;脊柱脑膜瘤
一、引言在神经外科领域,脊柱肿瘤的精准诊断与有效治疗一直是极具挑战性的课题。透明细胞脑膜瘤作为脑膜瘤的一种特殊亚型,其在脊柱部位的非硬脑膜来源表现更为罕见,临床医师对此认识相对不足。深入研究此类肿瘤的临床特征、治疗策略及预后因素,不仅有助于提升对罕见病的诊疗水平,更能为年轻患者提供更为精准、有效的医疗服务,改善其长期生存质量。本文通过报道一例典型病例并结合广泛的文献综述,旨在填补这一领域的知识空白,为同行提供参考借鉴。

术前影像;磁共振图像(a - e):矢状位 T1 加权像(a)、矢状位 T2 加权像(b)、显示强化的 T1 加权对比图像(c)、提示肿瘤内出血的短时反转恢复序列图像、冠状位 T2 加权像显示椎间孔延伸(e)、腰骶椎非增强计算机断层扫描(f)显示椎体前缘扇贝样改变及后部结构变薄 。
二、病例报告患者资料患者为一名 19 岁男性,因腰部疼痛伴下肢麻木无力数月就诊。既往无重大病史,家族史无遗传性神经系统疾病相关线索。影像学检查术前磁共振成像(MRI)显示腰骶部硬膜内一巨大占位性病变,呈等 T1、稍长 T2 信号,增强扫描明显强化,肿瘤头尾径≥2 个椎体节段,可见椎间孔延伸及椎体扇贝样改变(图 1),影像学表现与神经鞘瘤有一定相似性,初步鉴别诊断困难。手术过程与发现患者行后路椎板切除术,术中见肿瘤质地中等,血供较丰富,向椎间孔方向明显延伸,仔细分离后发现肿瘤与右侧 S1S2 神经根紧密相连,但令人意外的是,肿瘤无硬脑膜附着,这一特征与常见的硬脑膜来源脑膜瘤截然不同。手术团队凭借精湛技艺,完整切除肿瘤(GTR),过程顺利,术中出血得到有效控制。术后恢复与随访术后患者腰部疼痛及下肢症状逐渐缓解,神经系统功能恢复良好。术后 6 个月随访,行 MRI 检查,未见肿瘤复发迹象(图 2),患者生活质量显著提高,恢复正常学习与社交活动。
术后影像;术后 6 个月的随访磁共振图像(a - c)显示无疾病迹象及后方假性脑脊膜膨出。
三、文献综述流行病学特征通过对既往 19 例非硬脑膜来源脊柱 CCM 文献分析发现,该肿瘤具有明显的年龄与性别倾向。发病平均年龄仅 20.58 岁,年轻患者居多,且女性患者占比相对较高(63.16%)。从发病部位来看,腰骶部最为常见,高达 79% 的病例发生于此,提示该区域可能存在特定的解剖学或生物学因素,促使肿瘤易在此处发生发展。肿瘤形态学特点在肿瘤大小与累及范围方面,多数肿瘤(79%)头尾径≤2 个椎体节段,但仍有 21% 的肿瘤突破这一范围,可达≥2 个椎体节段,如本文所报道病例。这种大小差异可能影响手术难度、切除范围及预后判断,提示临床医师需根据具体情况制定个性化手术方案。治疗方式与预后关联治疗上,GTR 是主流选择,高达 95% 的患者接受了该术式,旨在彻底清除肿瘤组织,降低复发风险。然而,令人遗憾的是,仍有 26.14% 的患者出现复发,其中近 80%(4 例)在术后 6 个月内复发,最早复发时间为 STR 术后 2.3 个月,凸显即便看似根治性切除,肿瘤仍具有较高的生物学侵袭性,术后密切随访监测至关重要。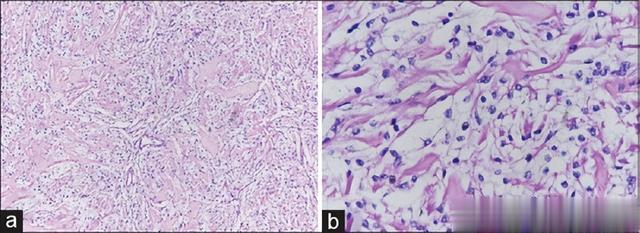
显微镜下组织病理学检查图像显示,圆形至多边形的脑膜上皮细胞具有丰富的透明细胞质,呈无序排列,血管周围及间质可见明显的块状胶原束(a,低倍视野),以及(b,高倍视野) 。
四、讨论诊断难点与影像学鉴别非硬脑膜来源脊柱 CCM 在诊断初期极具挑战性,其影像学表现与神经鞘瘤高度相似,如均可见椎间孔延伸、强化模式相近等,易误导临床判断。但细致分析仍可发现细微差异,如 CCM 可能更易出现椎体扇贝样改变,且肿瘤与神经根的附着方式、血供特点在术中探查时有别于神经鞘瘤。临床医师需综合多模态影像学资料、患者年龄、性别等因素,提高术前诊断准确率。手术策略优化鉴于肿瘤无硬脑膜附着但与神经根关系密切的特性,手术入路与操作技巧需精细调整。传统依赖硬脑膜分离的方法不再适用,术中应更加注重神经根的保护,避免损伤导致术后严重功能障碍。同时,对于血供丰富区域,术前栓塞或精细的止血技术应用可减少术中出血,保障手术视野清晰,提高肿瘤全切率。预后评估与长期随访意义尽管 GTR 是理想目标,但本研究及文献回顾均显示复发风险不容忽视。即使手术切除彻底,肿瘤细胞仍可能残留或通过脑脊液播散,因此,术后长期、规律的全神经系统随访不可或缺。定期 MRI 检查、神经系统功能评估,有助于早期发现复发迹象,及时干预,改善患者预后。五、结论巨大非硬脑膜来源腰骶部透明细胞脑膜瘤作为罕见脊柱肿瘤,给临床诊疗带来诸多挑战。通过本病例报告及文献综述,明确了其流行病学、临床特征、治疗难点与预后特点。临床医师应提高对该病的认识,综合运用精准诊断技术、优化手术策略,并强化术后随访,为患者提供最佳治疗方案,最大程度改善患者生存结局。未来,随着分子生物学、影像组学等技术发展,有望进一步揭示其发病机制,探索更有效的靶向治疗手段,填补当前治疗局限。
参考文献
Zhang H, Ma L, Shu C, Dong LQ, Ma YQ, Zhou Y. Spinal clear cell meningiomas: Clinical features and factors predicting recurrence. World Neurosurg. 2020;134:e1062–76. - PubMedLouis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organizationification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016;131:803–20. - PubMedLi J, Zhang S, Wang Q, Cheng J, Deng X, Wang Y, et al. Spinal clear cell meningioma: Clinical study with long-term follow-up in 12 patients. World Neurosurg. 2019;122:e415–26. - PubMedDe Verdelhan O, Haegelen C, Carsin-Nicol B, Riffaud L, Amlashi SF, Brassier G, et al. MR imaging features of spinal schwannomas and meningiomas. J Neuroradiol. 2005;32:42–9. - PubMedInoue T, Shitara S, Ozeki M, Nozawa A, Fukao T, Fukushima T. Hereditary clear cell meningiomas in a single family: Three-cases report. Acta Neurochir (Wien) 2018;160:2321–5. - PubMedKawasaki Y, Uchida S, Onishi K, Okanari K, Fujiki M. Pediatric nondura-based clear cell meningioma of the cauda equina: Case report and review of literature. Br J Neurosurg. 2020;34:215–8. - PubMedLi P, Yang Z, Wang Z, Zhou Q, Li S, Wang X, et al. Clinical features of clear cell meningioma: A retrospective study of 36 cases among 10,529 patients in a single institution. Acta Neurochir (Wien) 2016;158:67–76. - PubMedZhang J, Shrestha R, Li J, Shu J. An intracranial and intraspinal clear cell meningioma. Clin Neurol Neurosurg. 2013;115:371–4. - PubMedKobayashi Y, Nakamura M, Tsuji O, Iwanami A, Ishii K, Watanabe K, et al. Nondura-based clear cell meningioma of the cauda equina in an adult. J Orthop Sci. 2013;18:861–5. - PubMedKo JK, Choi BK, Cho WH, Choi CH. Non-dura based intaspinal clear cell meningioma. J Korean Neurosurg Soc. 2011;49:71–4. - PMC - PubMedPark SH, Hwang SK, Park YM. Intramedullary clear cell meningioma. Acta Neurochir (Wien) 2006;148:463–6. - PubMedEpstein NE, Drexler S, Schneider J. Clear cell meningioma of the cauda equina in an adult: Case report and literature review. J Spinal Disord Tech. 2005;18:539–43. - PubMedOviedo A, Pang D, Zovickian J, Smith M. Clear cell meningioma: Case report and review of the literature. Pediatr Dev Pathol. 2005;8:386–90. - PubMedChen MH, Chen SJ, Lin SM, Chen MH. A lumbar clear cell meningioma with foraminal extension in a renal transplant recipient. J Clin Neurosci. 2004;11:665–7. - PubMedPayano M, Kondo Y, Kashima K, Daa T, Yatsuka T, Kida H, et al. Two cases of nondura-based clear cell meningioma of the cauda equina. APMIS. 1924;112:141–7. - PubMedJallo GI, Kothbauer KF, Silvera VM, Epstein FJ. Intraspinal clear cell meningioma: Diagnosis and management: Report of two cases. Neurosurgery. 2001;48:218–21. - PubMedDubois A, Sévely A, Boetto S, Delisle MB, Manelfe C. Clear-cell meningioma of the cada equina. Neuroradiology. 1998;40:743–7. - PubMedMatsui H, Kanamori M, Abe Y, Sakai T, Wakaki K. Multifocal clear cell meningioma in the spine: A case report. Neurosurg Rev. 1998;21:171–3. - PubMedHoltzman RN, Jormark SC. Nondural-based lumbar clear cell meningioma. Case report. J Neurosurg. 1996;84:264–6. - PubMedZorludemir S, Scheithauer BW, Hirose T, van Houten C, Miller G, Meyer FB. Clear cell meningioma. A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol. 1995;19:493–505. - PubMedManivel JC, Sung JH. Pathology of meningiomas. Pathol Annu. 1990;25(Pt 2):159–92. - PubMedScheithauer BW. Tumors of the meninges: Proposed modifications of the World Health Organizationification. Acta Neuropathol. 1990;80:343–54. - PubMedKshettry VR, Hsieh JK, Ostrom QT, Kruchko C, Benzel EC, Barnholtz-Sloan JS. Descriptive epidemiology of spinal meningiomas in the United States. Spine (Phila Pa 1976). 2015;40:E886–9. - PubMedDuong LM, McCarthy BJ, McLendon RE, Dolecek TA, Kruchko C, Douglas LL, et al. Descriptive epidemiology of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors, United States, 2004-2007. Cancer. 2012;118:4220–7. - PMC - PubMedChamberlain MC, Glantz MJ. Cerebrospinal fluid-disseminated meningioma. Cancer. 2005;103:1427–30. - PubMedSmith MJ, Wallace AJ, Bennett C, Hasselblatt M, Elert-Dobkowska E, Evans LT, et al. Germline SMARCE1 mutations predispose to both spinal and cranial clear cell meningiomas. J Pathol. 2014;234:436–40. - PubMedCarrà S, Drigo P, Gardiman M, Perilongo G, Rigobello L. Clear-cell meningioma in a 22-month-old male: A case report and literature review. Pediatr Neurosurg. 2001;34:264–7. - PubMedTao X, Dong J, Hou Z, Hao S, Zhang J, Wu Z, et al. Clinical features, treatment, and prognostic factors of 56 intracranial and intraspinal clear cell meningiomas. World Neurosurg. 2018;111:e880–7. - PubMedYolcu YU, Goyal A, Alvi MA, Moinuddin FM, Bydon M. Trends in the utilization of radiotherapy for spinal meningiomas: Insights from the 2004-2015 National Cancer Database. Neurosurg Focus. 2019;46:E6. - PubMedPereira BJ, de Almeida AN, Paiva WS, Teixeira MJ, Marie SK. Impact of radiotherapy in atypical meningioma recurrence: Literature review. Neurosurg Rev. 2019;42:631–7. - PubMedHwang KL, Hwang WL, Bussière MR, Shih HA. The role of radiotherapy in the management of high-grade meningiomas. Chin Clin Oncol. 2017;6:S5. - PubMedKwee LE, Harhangi BS, Ponne GA, Kros JM, Dirven CM, Dammers R. Spinal meningiomas: Treatment outcome and long-term follow-up. Clin Neurol Neurosurg. 2020;198:106238. - PubMedWalcott BP, Nahed BV, Brastianos PK, Loeffler JS. Radiation treatment for WHO grade II and III meningiomas. Front Oncol. 2013;3:227. - PMC - PubMedWang C, Kaprealian TB, Suh JH, Kubicky CD, Ciporen JN, Chen Y, et al. Overall survival benefit associated with adjuvant radiotherapy in WHO grade II meningioma. Neuro Oncol. 2017;19:1263–70. - PMC - PubMedDi Franco R, Borzillo V, Ravo V, Falivene S, Romano FJ, Muto M, et al. Radiosurgery and stereotactic radiotherapy with cyberknife system for meningioma treatment. Neuroradiol J. 2018;31:18–26. - PMC - PubMed